Recovery after a football match: do we really understand what we are doing?
Written by Peter Joffe
Today the industry of football has gained enormous popularity. At the top level, elite players compete under enormous physical and psychological pressure. They often have to do that in different tournaments when a time for recovery between games is limited. Not to mention that they still need to train.
So, it is evident that recovery is a vital ingredient for successful performance and efficient training. For thousands of years, people engaged in sports, are looking for the best methods to restore their strength and endurance. Various recovery strategies are constantly emerging and evolving—however, our understanding of what we are doing and why, in my opinion, remains incomplete.
Before advising a specific recovery strategy, it is logical that it is necessary to understand the reasons for impairment in physical capacity after the game, the mechanism of their influence, and the proposed treatment mechanism. These are not easy questions. Nevertheless, it is worth to try to answer them. Efficient recovery gives a valuable advantage, while useless methods waste precious time and money. Moreover, as we will see later, recovery approaches that are good in one situation may be detrimental in another.
I am going to address the following problems in the present article:
First, I would like briefly to discuss game actions, which may lead to lasting impairment in performance.
Secondly, I will try to investigate the exact mechanism of how muscle damage develops.
Thirdly, I will consider how most popular recovery methods such as cold, massage, light exercise, etc. may facilitate or impair the recovery process. And finally, I will try to give some recommendations.
Game.
During the football match, players perform various actions, and each of them could lead to fatigue. The situation is even more complicated because these actions influence each other. For instance, you can be tired just making fifty sprints, but probably you will be tired more and differently if you are making those sprints together with tackles, turns, jumps, and 7-9 km jogging.
I have already discussed the reasons for fatigue during a football match (see article). The conclusion was that metabolites accumulating during intense actions, glycogen depletion in some muscle fibres, and exercise-induced muscle damage (EIMD) are the main factors. Some authors add dehydration, but it is probably the issue only when playing in the heat.
Here, unlike the mentioned article, I will discuss fatigue that lasts for several days and can impair performance in the next game. From this point of view, EIMD and glycogen depletion is our main concern. In my opinion, glycogen recovery should not be a problem, although this is important. I will cover this topic briefly. However, EIMD is, probably, a bigger issue, and I will discuss it in more detail.
EIMD.
During exercise, muscles can be damaged chemically and mechanically. The former is due to disturbances in homeostasis, whereas the latter is a consequence of mechanical stress. As usual, these two ways are interacting. For example, disorders in the chemical environment may lead to muscle fibres’ weakness, making a muscle more susceptible to damage. On the other hand, a mechanical load can change the permeability of cell membranes and ion channels’ functioning, consequently disturbing the chemical environment.
It is an interesting question of how we can measure muscle damage. Whereas most of the applying methods are relatively complicated and are used in laboratory settings, one indicator can be useful for practical coaches. That is a prolonged loss of strength and power, which can be measured by different physical tests. Most common are isokinetic and isometric strength tests, sprint, and countermovement jump (CJ).
Eccentric contractions.
From the different types of exercise, those that include eccentric contraction are associated with more severe muscle damage. Eccentric contraction (ECC) means that load is applied when a muscle is lengthening. Basically, it is forceful stretching. There are plenty of such contractions during sports games. Landing phases in running and jumping, braking actions during decelerations and sharp turns, antagonists muscles action while kicking the ball — all these are examples of ECC. These actions greatly influence long-lasting damage. For example, (Nedelec et al., 2014) found that muscle soreness and CMJ several days after play were more influenced by short, intense actions such as sharp turns, acceleration and deceleration than total work volume.
The reasons for increasing muscles vulnerability during ECC are still debated. Although metabolically ECC is less demanding than concentric contraction (CC), the applied force may be significantly higher. In addition to that, a pattern of muscles activation is different between ECC and CC. ECC recruits less muscle fibres thus load on individual fibre may be higher. Fast twitch fibres usually are damaged more during ECC. This may be due to they create optimal tension at shorter length compare to slow-twitch fibres (Proske & Morgan, 2001).
It means that while particular muscle length is still bearable for slow-twitch fibres it may be already critical for their fast-twitch peers thus, they may be damaged. Indeed, muscle lengthening is perhaps the most important damaging factor during ECC. When a muscle fibre is forcefully stretched beyond its optimal length, its resistance and elastic properties diminish (Lau, Blazevich, Newton, Wu, & Nosaka, 2015).
The extent of the damage depends on external and internal factors. Muscle lengthening, a magnitude of applied force, speed and duration of contractions are examples of external influences (Jonathan M Peake, Neubauer, Della Gatta, & Nosaka, 2016). Different people may also react differently to the same damaging exercise due to their genetic uniqueness and training adaptations. These are internal factors.
At the moment, we don’t understand exactly how ECC leads to muscle damage and loss of strength and power. However, it is worth discussing this problem deeper because recovery strategies may be dependent on that.
There are two main features which are evident after EIMD: mechanical disruption of sarcomeres (functional muscle unit) and malfunction of excitation-contraction (E-C) coupling system.
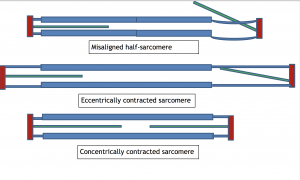
Supporters of the “popped sarcomeres” theory suggest that mechanical damage comes first (Proske & Morgan, 2001). They proposed that sarcomeres (or more exactly half-sarcomeres) within myofibril are not uniform. Some of them are weaker than others; thus, when an eccentrically applied load is sufficiently high, these half-sarcomeres become overstretched beyond their limit and may “pop out” from the position of overlapping filaments (Picture 1).
Picture 1. Popped sarcomere.
Top diagram – normal relaxed sarcomere. Middle diagram – normal concentrically contracted sarcomere. Bottom diagram – during eccentric contraction, right half-sarcomere popped from position of overlapping between myosin (thick blue rectangle) and actin (green rectangle). Trying to compensate for decreasing tension, left half-sarcomere contracts.
This may start chain-reaction when the load from knock-out sarcomeres is placed on their peers, and the next weakest follow their fate. During the relaxation phase, elastic elements attached to sarcomeres may pull back most of the popped units into the normal position; however, some remain displaced and damage spread to the adjacent fibres and cell membrane. Damage to the membranes leads to ionic disbalance, disturbance of E-C coupling system, and uncontrolled influx of Ca ions into the muscle cell. These are followed by local contracture, loss of muscle proteins, and, eventually, the death of some fibres and inflammation (Proske & Morgan, 2001).
Supporters of the E-C coupling theory suggest that, though a disruption in E-C coupling may start with a mechanical event, it may not be as severe as popped sarcomeres (Warren, Ingalls, Lowe, & Armstrong, 2002).
The opening of stretch-activated ionic channels may be enough to initiate the process. These channels can be activated even after a relatively mild but repeated stretching. That gradually changes the chemical balance. When ionic homeostasis becomes distracted, the E-C coupling system fails, and some fibres cannot contract.
Then, similar to popped sarcomeres version of events, this creates non-uniformity in tension and place additional strain on muscle membranes leading to their damage. An uncontrolled influx of extracellular Ca in intracellular space may initiate processes that lead to chemical degradation of the contractile proteins and magnify the damage (Kano, Sonobe, Inagaki, Sudo, & Poole, 2012).
I do not have enough expertise to judge which theory is correct though my intuition tells me that both may be accurate depending on circumstances.
It is known that muscle damage can occur not only from high-magnitude ECC ( e.g. plyometrics) but after low-magnitude and long-duration contractions like, for example, long-distance run (Nosaka et al., 2010; Gomez et al., 2002).
Symptoms of EIMD are similar, and both events may cause inflammation and loss of strength but, possibly, in the latter case, individual eccentric contraction doesn’t overstretch sarcomeres. Here E-C coupling variant looks more plausible. Firstly stretch-activated channels may be activated, disrupting normal E-C coupling, which triggers a chain of events, eventually leading to fibres damage. However, in case of more intense eccentric actions, like rapid turns, decelerations, landings, etc., popped sarcomeres may be the trigger.
In sports games, we have a mix of different activities that can add complexity to understanding the order of events. Imagine a football cup game which goes to extra-time. This game lasts 120 minutes; some players may cover up to 15 kilometres distance while doing a lot of intense actions. What came first in this scenario is hard to say. Does the player overstretch sarcomeres first and then aggregates damage with the overall load? Or a lot of running makes him more susceptible to mechanical damage? At the moment, we cannot say for sure. However, in any case, the player may end up with damaged and disrupted fibres, local contracture, and the start of inflammation.
Soreness and tenderness.
EIMD can promote (though not always) soreness and tenderness, which can impair an athlete’s recovery psychologically and functionally. Interestingly, this unpleasant feeling and strength loss peaks after 24-48 hours after exercise; thus, it even has a special name: delayed onset of muscle soreness —DOMS. The nature of DOMS is not completely understood and more likely is very complex. What is the exact reason for soreness? Why it begins later and peaks after a couple of days?
The most common explanation is that in response to stimulation and damage, myofibrils produce signal proteins that initiate a very complex response that ultimately eliminates damage. However, some parts of this response may be inflammation, oedema, and swelling, as well as decreased pain threshold (Hyldahl & Hubal, 2014). These conditions may gradually increase after the cessation of the exercise and create DOMS. For the process of recovery, inflammation is a particular interesting factor.
Inflammation.
Inflammation is part of the adaptation process in training. It begins almost immediately after the end of exercise and may continue long after that. In simple words, the role of inflammation is cleaning the “debris” and rebuilding the damaged muscles (Urso, 1985, Tidball, 2005). In this sense, it is necessary for normal recovery. However, if the inflammation process goes too far, as it may be in the case of severe damage, it may hurt even healthy muscle tissues, thus becoming dangerous.
The answer to the question of the usefulness of inflammation is very important because fighting it is one of the main priorities of the modern recovery ideology. So, is it an enemy or a friend? Well, we don’t have a simple answer. Inflammation is a very complex and finely regulated process. Many authors claim that some anti-inflammation interventions ( e.g. cold and medication) actually impair training adaptations. Ideally, it would be great to limit its damaging influence, whereas not to interfere with the positive (Toumi & Best, 2003). Unfortunately, contemporary recovery methods cannot act with such precision.
Practical advice depends on whether anti-inflammation intervention is needed or not. We have to consider how serious actual damage is and how much time we have for recovery. It is probably unnecessary to fight inflammation during the training period, and if muscle damage is not severe. However, if you need quick recovery between consecutive games and muscle damage is considered severe, some anti-information strategies are justified.
“… data seem to indicate that the primary inflammatory phase is essential for the induction of signals that control tissue regeneration. However, attenuating the secondary inflammatory phase and the subsequent secondary muscle injury may be an effective treatment approach”(Urso, 1985).
Summary of EIMD.
Physical exercise, especially ECC, may lead to muscle damage. This impairment may be caused by the interaction between ionic homeostasis disturbances and direct mechanical damage. The manifestation of EIMD may be the loss of strength and power, muscle tightness, soreness, and swelling.
That can last for days and influence performance in the next game or training session. However, some “unpleasant” sensations after exercise and mild inflammation may be signs of positive recovery and adaptation. Exercise professionals have to consider the whole picture when choosing recovery strategies for their athletes.
Recovery.
There are a few most popular recovery methods which I would like to discuss.
Cold water immersion.
Between widespread recovery technics, cold water immersion (CWI) is probably the most popular among professional athletes. The keywords here are “cold” and “immersion”.
Cold is supposed to restrict blood flow to damaged muscles, which is considered beneficial for reducing inflammation, oedema, and swelling. Additionally, it decreases muscle’s temperature, which might be helpful for attenuation of post-exercise oxidative damage.
Water immersion deep, at the neck level, creates hydrostatic pressure, which can increase blood flow from the periphery towards centre, hence enhancing metabolite clearance from muscles.
To investigate what is beneficial in CWI, we can try to look at cold and immersion separately.
There is another popular, though much more expensive technique for cooling without immersion – cryo-chamber. In this device, an athlete is exposed to extremely cold air ( up to-130 C ) for 3 min. Most researchers found a very limited effect of cryo-chambers on recovery (Costello et al., 2015). Can we conclude that cold doesn’t help? Well, perhaps a short time of exposure and lower (compare to water) thermal capacity of air are the main reasons for the relative inefficiency of cryo-chambers, not the inefficiency of cold per se. Cold is more efficient when applied to the whole body than local application to exercising muscles (Poppendieck, Faude, Wegmann, & Meyer, 2013). This can be seen as an affirmation that reducing local inflammation is not the only effect of cold.
When we look at immersion in the absence of cold, neutral and cool water has some positive impact. That confirms the idea that, regardless of the cold, immersion itself is a good thing to do. Wilcock et al. suggested using cool and thermoneutral water as a preferable option to cold water unless some more severe damage has occurred (Wilcock, Cronin, & Hing, 2006).
Generally, the literature shows some positive effects of CWI on soreness and pain perception, though a minimal effect on performance recovery (Leeder, Gissane, van Someren, Gregson, & Howatson, 2011; Kositsky, Cronin, & Avela, 2017). Typical recommendations are water temperature 10-15 degrees C, immersion for 10-15 min at the neck level. Better to do this immediately after the game and repeat on the following days (Versey, Halson, & Dawson, 2013).
However, there are a few issues with CWI.
First of all, it is an unpleasant procedure, and not all athletes like it. Due to benefits from CWI are limited and debatable, do we really have to insist that a player, who doesn’t like CWI, dives into the cold bath? I am not convinced. Federer: I am the guy who does not do cold bath.
Probably, even the more important question is that exposure to cold may interrupt normal muscles rebuilding progression. Inflammation and oxidative stress initiate some signalling processes that ultimately push the body to repair the damage with even stronger and more adapted muscles. Inflammation per se is necessary for cleaning the debris from the damaged tissues. As cold is supposed to fight inflammation and oxidative stress, it can actually impair rebuilding and adaptation. Indeed, many authors found CWI between training sessions detrimental to strength and endurance gains (Roberts et al., 2015). So we should be careful and think twice before using CWI in a particular situation.
Conclusion:
“Individuals who use strength training to improve athletic performance, recover from injury or maintain their health should, therefore, reconsider whether to use cold water immersion as an adjuvant to their training”(Yamane et al., 2006).
“Periodic use of cold water immersion may assist athletes when they need to recover quickly between training sessions or competitive events. However, in the long term, regular cold water immersion appears to be detrimental to developing muscle strength and hypertrophy “(J. M. Peake et al., 2017).
I do not recommend CWI during training because long- term adaptation may be compromised.
Spa-treatment.
Spa treatment may provide some alternative for CWI. At least it is not so unpleasant. Usually, it combines short cold water immersion or shower with exposure to heat (sauna or hot shower). That can be supplemented with hydromassage (jacuzzi).
The idea is that changing between cold and hot temperature leads to alterations between vasoconstriction and vasodilation, resulting in muscle pumping effect, increasing metabolism, and by-products. Buchheit et al. found a positive effect of spa-treatment on performance in young football players (Buchheit, Horobeanu, Mendez-Villanueva, Simpson, & Bourdon, 2011).
Massage.
Massage is a popular recovery method and probably the oldest one.
Despite that, we perhaps don’t exactly understand why we are using it for recovery.
The most common explanation is that massage increases blood flow in the fatigued muscles, thus speeding up metabolite clearance. That is doubtful. Massage probably doesn’t increase blood flow, and even if it does, then light exercise can do this much better.
Another idea is that massage can help to re-align disrupted muscle fibres and to relieve local contracture. Possibly it may be the case; however, to my knowledge, there is no scientific evidence for this (Weerapong, Hume, & Kolt, 2005).
Crane and colleagues suggested another explanation of possible benefits from massage, which was supported by scientific research. Mechanical stretch and strain during massage activate some signalling proteins which promote anti-inflammation response, mitochondrial biogenesis, and indirectly facilitate metabolic recovery (Crane et al., 2012).
Researches on benefits from massage are equivocal. Generally, there is no effect on performance recovery. Some positive effects on soreness and perception of recovery were found, possibly due to the placebo effect ( Dawson, & Tiidus, 2004). Massage is mostly recommended immediately after the game. That makes sense if we consider the anti-inflammatory effect and fibres re-aligning. However, it is technically difficult to give massage to all players after the match.
Moreover, in my opinion, conceptually massage is not compatible with CWI, because the latter actually aims to decrease blood flow and to cool down muscles. What we really want: to decrease muscle temperature and blood flow (CWI) or increase those (massage)? We have to decide. Thus in practice, it may be better if players received a massage next day after the game or instead of CWI if it is given immediately after the game.
Conclusion:
“On average, the effects of massage on performance recovery are limited but can be relevant under certain circumstances” (Poppendieck et al., 2016).
Active recovery.
The main idea of doing light exercise after the game is to increase metabolism in damaged muscles, thus speeding up recovery. It looks plausible. This notion may be supported by increasing lactate clearance speed in active recovery conditions compared to passive rest. Blood lactate is not a reason for damage and fatigue, and perhaps even is not a reliable indicator of metabolic disturbance (Minas, Radak, & Takeda, 2017). However, we may assume that if its clearance speeds up, then, possibly, other by-products are removed faster as well.
Other benefits of active recovery are the possibility of re-aligning fibres and natural “muscle pumping,” which can reduce swelling and oedema. In reality, the athlete often feels better after starting the active recovery session but after its cessation, tenderness and soreness usually return (Armstrong, 1984).
There are three questions: what to do, when and how much. Usually, players have not a lot of time after the game so active recovery is given to them the next day. Another reason for avoiding exercise immediately after the game is that it may impair glycogen restoration (Barnett, 2006).
Light jogging is (or was) the most popular form of active recovery. However, some coaches don’t want to aggravate the damage by the impact forces associated with running, so they prefer a bike. The usual duration is 20-40 min, intensity around 60-70% of VO2max.
As it often happens, studies give equivocal results for the effectiveness of active recovery. Usually, it is better than doing nothing but shows no advantage compare to other recovery methods (Barnett, 2006).
Conclusion:
Active recovery should be performed on the next day, and it is probably better to do exercises other than running.
Compressive garments.
This method aims to create pressure on exercised limbs, thus facilitating blood flow, venous return, and removal of excessive fluid. That should improve recovery. We already meet this idea when discussed the hydrostatic effect of water immersion. An advantage of the compressive garment is that you can wear them much longer than sitting in the pool. Usually, players do this for a few hours.
The one problem with the compressor garments is that pressure should gradually decrease from the limb’s distal part to the proximal one. It is not that all models have been achieved. Another issue is the posture. Different body positions may result in different pressure patterns (Brophy-Williams, Driller, Shing, Fell, & Halson, 2015). Since the compression garments should be worn for a relatively long time, it is difficult to require players to be in certain positions.
Despite the mentioned limitations, generally, CG show positive though a small, effect on recovery (Marques-Jimenez, Calleja-Gonzalez, Arratibel, Delextrat, & Terrados, 2016; Hill, Howatson, Van Someren, Leeder, & Pedlar, 2013). Maybe it is a mostly psychological effect, but there is no harm to wear it for some time.
Conclusion:
Generally, CGs are good but:
“The pressure applied by sports compression garments is significantly affected by garment type, size and posture assumed by the wearer” ( Brophy-Williams, Driller, Shing, Fell, & Halson, 2015).
Stretching.
The rationale for using stretching after EIMD is that damaged muscles can be spasmed (Herbert & de Noronha, 2007). Probably, in reality, it is not the case if we refer to spasm as massive, painful, and uncontrolled contraction, something similar to cramps. EIMD may cause local contracture and shortened half-sarcomeres but this is not a whole-muscle spasm. Herbert et al. pointed out that our current understanding of EIMD leaves no place for stretching as a cure for muscle damage.
In my experience, stretching may provide some temporal relief. Perhaps this is because misaligned fibres, which tear adjacent tissues, may be pulled away. However, stretching does not fix disruption; hence after stretch, stiffness returns. Nevertheless, some players feel better doing stretching after the game. I don’t see why it may be bad, although some coaches argue that there is a risk of aggravating ECC damage. I don’t think so if you are doing stretch carefully. Long-term consistent stretching may also provide some advantage by making muscles more adaptive to tension at a longer length. That may be a good adaptation for ECC.
Conclusion:
Stretching is not an immediate cure of EIMD but may be beneficial for a long- term adaptation.
Hydration and food consumption.
I already discussed hydration problems in details (see article). Dehydration may be an issue during the game, especially in the hot environment; however, in my opinion, 24 hours between the games should be enough to restore water and minerals balance. I don’t think I can add something at the moment.
Considering energy store restoration, it is very important to reinstate glycogen reserves and supply repairing muscles with proteins.
An appropriate dietary routine can enhance the synthesis that occurs over the short-term. The prevailing opinion is that there is some “window of opportunity” immediately after the game when carbohydrates and proteins are digested better. For example, Barnett suggested consuming 1.2 g of carbohydrates per kg of body weight every hour at regular intervals immediately after and up to 5 hours post-exercise (Barnett, 2006).
Perhaps, a special window does not exist (Aragon & Schoenfeld, 2013), but there is no harm to start the restoration of energy reserves and proteins as soon as possible. Many teams use milkshakes immediately after the match. Additionally, the early start may help with more proportional food consumption.
Healthy food can provide all necessary for reinstatement of glycogen stores, proteins, fluid, and minerals. In my opinion, no special interventions are needed if games are separated more than 48 hours.
Conclusion:
“Current recommendations are that ingesting 0.8–1.2 g CHO/kg/h and 0.2–0. 4 g. protein/kg/h, preferably in the early recovery period, with a minimum content of 20g high-quality protein, may enhance the recovery after EIMD” (Sousa, Teixeira, & Soares, 2014).
Anti-inflammation and anti-oxidants drugs.
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used among the athletic population. The aim is to reduce inflammation and pain. Different types and doses of NSAIDs are used with different reported effects.
The majority of research generally shows that these medications have little effect on recovery from EIMD (Connolly, Sayers, & McHugh, 2003). Moreover, as I already discussed in the “Inflammation” section of this article, anti-inflammation drugs, as pointed out Schoenfeld, may ”blunt more than pain” (B.Schoenfeld,2017). They can impair training gains by altering the body response to exercise. (J. M. Peake et al., 1985). Lilja et al. found that high-dose anti-inflammatory drugs compromise muscle strength and hypertrophic adaptations to resistance training. (Lilja et al., 2018). Also, they may have some unfavourable side-effects such as gastrointestinal distress, renal disorders and hypertension. Stronger NSAIDs may have more harmful side-effects and their use should be limited (Connolly, et al., 2003).
Antioxidants.
During exercise, the body produced chemically active free radicals contained oxygen. Reactive oxygen species (ROS) are part of the normal response to exercise; however, they may be produced in great numbers and contribute to muscle damage when unaccustomed. It is called oxidative stress. I already mentioned one of the strategies to reduce ROS production by lowering metabolism when discussed the effect of cold therapy.
Another way is to use antioxidant vitamins, mainly C (ascorbic acid) and E (tocopherol), which can clean ROS out of the body. That makes such vitamins hugely popular among athletes who routinely use them in high doses.
However, in their comprehensive review (McGinley, Shafat, & Donnelly, 2009), McGinley et al. noted that there is little evidence of actual benefits of antioxidant supplementation for EIMD prevention and recovery. Moreover, this may damp ROS cellular signalling function and impair training adaptation. Authors even mentioned that long-term use of high doses of vitamin E might increase all-cause mortality (McGinley, et al., 2009).
I have to honestly confess that I am probably biased against the use of medication and vitamin supplements. In my opinion, nature, for millions of years of evolution, has created a sufficiently effective mechanism that balances complicated recovery processes in the human body. There is no need to interfere with this process if you are unsure about benefits, long-term influences, and harmful side effects.
Conclusion:
Normal, healthy, and balanced food can provide all the necessary ingredients for training and recovery. There are plenty of studies supporting the notion that natural sources of vitamins and antioxidants such as cherry juice, pomegranates, citruses, etc., are preferable options compared to synthetic products. At least it is difficult to overdose them. Thus, if there are no pathological problems and severe vitamins/minerals deficits, it would be better to stay away from drugs.
Why studies are always inconclusive and contradictory?
The main issue with researching recovery is that analysis of literature often results in conflicting and equivocal conclusions. Why is it so?
Well, first of all, the human organism is a very complex system. There are no two identical human bodies in the World, so when we investigate which recovery method is better, we have to consider that result maybe just due to the differences in people, not the differences in approaches.
Even if you compare different methods on the same person, it is difficult to control unrelated influences that may bias the research results. Different damage protocols, small nuances in recovery procedures, and even athlete beliefs may greatly influence the study’s outcome. And this is what often happened.
Secondly, if we investigate damage and recovery in the laboratory, perhaps we may control as many unrelated effects as possible; however, are laboratory settings comprehensively reflecting real game conditions?
On the other hand, while investigating damage and recovery after the real game, we may find ourselves in a very complex and variable environment; thus, we cannot be sure what really influenced the study’s outcome. It isn’t easy to control and separate all factors and make robust, scientific conclusions (Nedelec et al., 2012).
So, what can we do? Perhaps we have to rely on probability, common sense and hope that our better understanding of the human body will eventually help us. We can advise athletes on recovery, but, at the same time, it is necessary to listen to them. Recovery should be individual and specific for every player and take into consideration particular circumstances.
Restoration of order.
In my opinion, if something is not fixed, it continues to cause damage. I personally had this unpleasant experience with my injuries (non-severe dislocations). Though they were basically mechanical misalignments, they caused pain and inflammation, which healed relatively quickly when the problem was fixed.
I suppose that the same may be true for EIMD. If exercise results in mechanical disturbances, it would be better to fix them first.
Of course, exercise-induced injury is different from the traumatic injury of muscles. It is not a complete and massive rupture of muscle’s fibres or muscle/tendon sprain. Sarcomere disruption does not extend the length of a myofibril and usually does not extend across a whole muscle fiber (Connolly, et al., 2003). In fact, adjacent fibers may be relatively normal. Very often, there are just some distortions and misalignment. However, if this is not fixed, it may cause a prolonged decrease in function and trigger further damage.
It is perhaps why all, discussed above methods sometimes have a positive effect and sometimes have not. Cold may fight inflammation, but it cannot fix popped sarcomeres. Stretching can provide transitional relief, but it unlikely to re-aligns disrupted fibres. Massage and active recovery probably may be somehow helpful in this aspect, but they are not particularly useful. Misaligned fibres and popped sarcomeres may continue to tear themselves and adjacent tissues hence delay recovery.
I suggest the following method to confront the problem.
First of all, we need to drag misaligned elements back from the sites of tearing. We can try to do this by lengthening muscle under tension. Yes, basically, this is ECC but differently from the “chaotic” ECC during the game, in this case, lengthening and tension are steady, smooth, and controlled. It is different from passive, static stretching as well because you are not trying to relax muscles, and they are not static ( they are lengthening). The range of muscle elongation is individual and depends on the feeling of pain and discomfort. However, the aim is full range. During this movement, muscle fibres and connective tissues, and elastic elements elongate as well; hence their traction forces disrupted elements back into a natural position.
From this position, you move backward, performing a concentric contraction with the same load, so that now the tension of the contracted fibres and the recoil of elastic elements return the disrupted parts to their “slots”. (Picture 2).
Picture 2. Re-aligning of popped half-sarcomere.
Top diagram – popped right half-sarcomere. (Proske & Morgan, 2001) proposed that, due to misalignments, actin (green rectangle) may butt up against myosin (thick blue rectangle). Middle diagram – controlled eccentric contraction pull away actin from site of tearing with myosin. Bottom diagram – concentric contraction and elastic recoil pulled actin back between myosin filaments.
It is not a strength exercise per se but rather some kind of gymnastics, so the number of repetitions and load shouldn’t be high. For example, I recommended to my students to do 2 sets of 5-8 reps immediately after the game. You may feel some discomfort during first rep but it becomes less to the fifth. It feels much better in the second set. I advise repeating this routine a few times through the next day/s.
The main muscle groups are quadriceps, hamstring, calf and low back. Perhaps some exercises are a bit unusual but I managed to find examples on YouTube. It is very important to note that before doing this gymnastics player should get used to these exercises and be able to perform them even at the greater load. Additionally, I want to emphasise that I am suggesting the idea and do not insist on particular exercises. I am sure that professionals, who will read this article, may find their own forms and workouts.
Exercise examples:
Quadriceps and knees:
Hamstring
Calf
Low back
You can use help from your team –mate instead of barbells
A cold bath or spa-therapy may supplement these exercises (perform gymnastics first) and other active recovery exercises like, for instance, bike or aqua-gymnastics (next day).
I understand that the suggested method is rather speculative. I cannot conduct a robust experiment to prove this idea, and I am not sure that muscles work exactly as I think. However, in my opinion, it is worth to try. First of all, it has some logic behind it. Secondly, it is not time-consuming. And finally, it should not be harmful because most researchers agree that light, eccentric exercise doesn’t aggregate EIMD (Connolly, et al., 2003).
Example of recovery procedure after a football game (evening).
Immediately after:
1. Gymnastics
2. Light snack
3. Spa-therapy/cold bath
4. Compressive garments.
5. Additional food consumption with anti-oxidant/anti-inflammation fruits and juices.
6. Relaxation/meditation and sleep.
Next day
1. Active recovery (bike, swimming pool). Maybe light strength training for upper body.
2. Gymnastic
3. Spa-therapy
4. Massage
5. Normal food throughout the day. Maybe with some increase in protein and carbohydrate content if energy expenditure was significant.
Prevention of EIMD.
And the last thing I want to say is that it is always better to prevent damage than to deal with its consequences. In this sense, possibly, the best method for adaptation to eccentric contraction is… eccentric contraction (Cleak & Eston, 1992). Though physical conditioning specialists always pay attention to strength training for preventing injuries, not all of them understand the importance of eccentric training. Specific eccentric training may facilitate vital muscle changes such as an increased number of sarcomeres in fibre (Proske & Morgan, 2001) and decreasing lengthening during ECC (Lau, et al., 2015). That can attenuate or even prevent muscle damage.
Summary.
During the game, exercised muscles may be damaged. The extent of EIMD depends on activity patterns, duration, intensity, and individual genetics and training adaptations.
The main objectives of recovery are:
1. To prevent further damage.
2. To restore homeostasis and muscle functions.
To solve these problems, we have to consider mainly two things: fibres disarrangement and inflammation. If the former won’t be fixed it may aggravate the latter. So I am suggesting special gymnastics to fix misalignment first.
Mild inflammation, soreness, and pain can be part of adaptation and recovery. Therefore, I recommend: do not fight them unless there is a reason to consider it serious and during training periods. Time heals.
CWI may be part of recovery during competitive periods when the next game will be soon after the previous one. However, it should be considered individually and, if a player doesn’t like cold water, it may be substituted by spa-treatment and massage.
Healthy food can provide all necessary for the restoration of glycogen stores, fluid, minerals and vitamins. In my opinion, no special dieting interventions are needed (except increasing glycogen and protein content) if games are separated for more than 48 hours.
The beliefs of the players play an important role in recovery. Thus, even if some interventions do not provide significant and scientifically proven benefits, but at least they do not harm, and players love and trust them, they should be used.
No special recovery procedures are required and some may even be harmful to young players. First, at this age, EIMD is usually less severe. Secondly, young athletes have yet to develop strength, endurance and speed even during competitive periods. EIMD is part of the training and adaptation process. There is no need to interrupt this.
Eccentric exercises should be part of strength training because they promote specific adaptation for EIMD.
.
The BASES ( British Association of Sport and Exercise Sciences) Expert Statement on Athletic Recovery Strategies.
• Determine if a strategy is necessary or whether recovery can be attained without intervention.
• Understand the training and competition stressors causing reductions in performance and delayed recovery before applying the intervention.
• Determine the relative importance of short-term recovery and long-term adaptation; consider how the concept of hormesis∗ could be applied.
• The importance of athlete belief in the intervention should not be underestimated.
• Research should combine multidisciplinary, mechanistic and performance approaches to elucidate the impact of recovery strategies on recovery and adaptation.
(Leeder & van Someren FBASES)
∗ Hormesis is a biological phenomenon whereby a beneficial effect (improved health, stress tolerance, growth or longevity) results from exposure to low doses of an agent that is otherwise toxic or lethal when given at higher doses ( https://gettingstronger.org/hormesis )
References.
Aragon, A. A., & Schoenfeld, B. J. (2013). Nutrient timing revisited: is there a post-exercise anabolic window? J Int Soc Sports Nutr, 10(1), 1550-2783.
Armstrong, R. (1984). Mechanisms of exercise-induced delayed onset muscular soreness: a brief review. Medicine and science in sports and exercise, 16(6), 529-538.
Barnett, A. (2006). Using recovery modalities between training sessions in elite athletes: does it help? Sports Med, 36(9), 781-796.
Brophy-Williams, N., Driller, M. W., Shing, C. M., Fell, J. W., & Halson, S. L. (2015). Confounding compression: the effects of posture, sizing and garment type on measured interface pressure in sports compression clothing. J Sports Sci, 33(13), 1403-1410.
Buchheit, M., Horobeanu, C., Mendez-Villanueva, A., Simpson, B. M., & Bourdon, P. C. (2011). Effects of age and spa treatment on match running performance over two consecutive games in highly trained young soccer players. J Sports Sci, 29(6), 591-598.
Cleak, M., & Eston, R. (1992). Delayed onset muscle soreness: mechanisms and management. Journal of Sports Sciences, 10(4), 325-341.
Connolly, D. A., Sayers, S. E., & McHugh, M. P. (2003). Treatment and prevention of delayed onset muscle soreness. The Journal of Strength & Conditioning Research, 17(1), 197-208.
Costello, J. T., Baker, P. R., Minett, G. M., Bieuzen, F., Stewart, I. B., & Bleakley, C. (2015). Whole-body cryotherapy (extreme cold air exposure) for preventing and treating muscle soreness after exercise in adults. Cochrane Database Syst Rev, 18(9).
Crane, J. D., Ogborn, D. I., Cupido, C., Melov, S., Hubbard, A., Bourgeois, J. M., & Tarnopolsky, M. A. (2012). Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Science translational medicine, 4(119), 119ra113-119ra113.
Dawson, L. G., Dawson, K. A., & Tiidus, P. M. (2004). Evaluating the influence of massage on leg strength, swelling, and pain following a half-marathon. Journal of sports science & medicine, 3(YISI 1), 37.
Gomez, A. L., Radzwich, R. J., Denegar, C. R., Volek, J. S., Rubin, M. R., Bush, J. A., . . . Kraemer, W. J. (2002). The effects of a 10-kilometer run on muscle strength and power. J Strength Cond Res, 16(2), 184-191.
Herbert, R. D., & de Noronha, M. (2007). Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev, 17(4).
Hill, J., Howatson, G., Van Someren, K., Leeder, J., & Pedlar, C. (2013). Compression garments and recovery from exercise-induced muscle damage: a meta-analysis. Br J Sports Med, bjsports-2013-092456.
Hyldahl, R. D., & Hubal, M. J. (2014). Lengthening our perspective: morphological, cellular, and molecular responses to eccentric exercise. Muscle & nerve, 49(2), 155-170.
Kano, Y., Sonobe, T., Inagaki, T., Sudo, M., & Poole, D. C. (2012). Mechanisms of exercise-induced muscle damage and fatigue: Intracellular calcium accumulation. The Journal of Physical Fitness and Sports Medicine, 1(3), 505-512.
Kositsky, A., Cronin, N., & Avela, J. (2017). The effect of cold water immersion on medial gastrocnemius muscle architecture and performance post-exhaustive stretch-shortening cycle exercise.
Lau, W. Y., Blazevich, A. J., Newton, M. J., Wu, S. S. X., & Nosaka, K. (2015). Reduced muscle lengthening during eccentric contractions as a mechanism underpinning the repeated-bout effect. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 308(10), R879-R886.
Leeder, J., Gissane, C., van Someren, K., Gregson, W., & Howatson, G. (2011). Cold water immersion and recovery from strenuous exercise: a meta-analysis. Br J Sports Med, bjsports-2011-090061.
Leeder, J., & van Someren FBASES, K. The BASES Expert Statement on Athletic Recovery Strategies.
Lilja, M., Mandic, M., Apro, W., Melin, M., Olsson, K., Rosenborg, S., . . . Lundberg, T. R. (2018). High doses of anti-inflammatory drugs compromise muscle strength and hypertrophic adaptations to resistance training in young adults. Acta Physiol, 222(2), 16.
Marques-Jimenez, D., Calleja-Gonzalez, J., Arratibel, I., Delextrat, A., & Terrados, N. (2016). Are compression garments effective for the recovery of exercise-induced muscle damage? A systematic review with meta-analysis. Physiol Behav, 153, 133-148.
McGinley, C., Shafat, A., & Donnelly, A. E. (2009). Does antioxidant vitamin supplementation protect against muscle damage? Sports Med, 39(12), 1011-1032.
Minas, H., Radak, Z., & Takeda, M. (2017). Active Recovery between Interval Bouts Reduces Blood Lactate While Improving Subsequent Exercise Performance in Trained Men (Vol. 5).
Nedelec, M., McCall, A., Carling, C., Legall, F., Berthoin, S., & Dupont, G. (2014). The influence of soccer playing actions on the recovery kinetics after a soccer match. The Journal of Strength & Conditioning Research, 28(6), 1517-1523.
Nedelec, M., McCall, A., Carling, C., Legall, F., Berthoin, S., & Dupont, G. (2012). Recovery in soccer. Sports Medicine, 42(12), 997-1015.
Nosaka, K., Abbiss, C., Watson, G., Wall, B., Suzuki, K., & Laursen, P. (2010). Recovery following an Ironman triathlon: A case study (Vol. 10).
Peake, J. M., Markworth, J. F., Nosaka, K., Raastad, T., Wadley, G. D., & Coffey, V. G. (1985). Modulating exercise-induced hormesis: Does less equal more? J Appl Physiol, 119(3), 172-189.
Peake, J. M., Neubauer, O., Della Gatta, P. A., & Nosaka, K. (2016). Muscle damage and inflammation during recovery from exercise. Journal of Applied Physiology, 122(3), 559-570.
Peake, J. M., Roberts, L. A., Figueiredo, V. C., Egner, I., Krog, S., Aas, S. N., . . . Raastad, T. (2017). The effects of cold water immersion and active recovery on inflammation and cell stress responses in human skeletal muscle after resistance exercise. J Physiol, 595(3), 695-711.
Poppendieck, W., Faude, O., Wegmann, M., & Meyer, T. (2013). Cooling and performance recovery of trained athletes: a meta-analytical review. International Journal of Sports Physiology and Performance, 8(3), 227-242.
Poppendieck, W., Wegmann, M., Ferrauti, A., Kellmann, M., Pfeiffer, M., & Meyer, T. (2016). Massage and performance recovery: a meta-analytical review. Sports Medicine, 46(2), 183-204.
Proske, U., & Morgan, D. (2001). Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. The Journal of Physiology, 537(2), 333-345.
Roberts, L. A., Raastad, T., Markworth, J. F., Figueiredo, V. C., Egner, I. M., Shield, A., . . . Peake, J. M. (2015). Post-exercise cold water immersion attenuates acute anabolic signalling and long-term adaptations in muscle to strength training. J Physiol, 593(18), 4285-4301.
Schoenfeld, B. J. Non-steroidal anti-inflammatory drugs may blunt more than pain: Acta Physiol (Oxf). 2018 Feb;222(2). doi: 10.1111/apha.12990. Epub 2017 Nov 30.
Sousa, M., Teixeira, V. H., & Soares, J. (2014). Dietary strategies to recover from exercise-induced muscle damage. Int J Food Sci Nutr, 65(2), 151-163.
Tidball, J. G. (2005). Inflammatory processes in muscle injury and repair. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 288(2), R345-R353.
Toumi, H., & Best, T. (2003). The inflammatory response: friend or enemy for muscle injury? British Journal of Sports Medicine, 37(4), 284-286. doi: 10.1136/bjsm.37.4.284
Urso, M. L. (1985). Anti-inflammatory interventions and skeletal muscle injury: benefit or detriment? J Appl Physiol, 115(6), 920-928.
Versey, N. G., Halson, S. L., & Dawson, B. T. (2013). Water immersion recovery for athletes: effect on exercise performance and practical recommendations. Sports Medicine, 43(11), 1101-1130.
Warren, G. L., Ingalls, C. P., Lowe, D. A., & Armstrong, R. B. (2002). What mechanisms contribute to the strength loss that occurs during and in the recovery from skeletal muscle injury? J Orthop Sports Phys Ther, 32(2), 58-64.
Weerapong, P., Hume, P. A., & Kolt, G. S. (2005). The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Medicine, 35(3), 235-256.
Wilcock, I. M., Cronin, J. B., & Hing, W. A. (2006). Physiological response to water immersion. Sports Medicine, 36(9), 747-765.
Yamane, M., Teruya, H., Nakano, M., Ogai, R., Ohnishi, N., & Kosaka, M. (2006). Post-exercise leg and forearm flexor muscle cooling in humans attenuates endurance and resistance training effects on muscle performance and on circulatory adaptation. Eur J Appl Physiol, 96(5), 572-580.