“The importance of breathing need hardly be stressed. It provides the oxygen for the metabolic processes; literally it supports the fires of life. But breath as “pneuma” is also the spirit or soul. We live in an ocean of air like fish in a body of water. By our breathing we are attuned to our atmosphere. If we inhibit our breathing we isolate ourselves from the medium in which we exist”.
“The importance of breathing need hardly be stressed. It provides the oxygen for the metabolic processes; literally it supports the fires of life. But breath as “pneuma” is also the spirit or soul. We live in an ocean of air like fish in a body of water. By our breathing we are attuned to our atmosphere. If we inhibit our breathing we isolate ourselves from the medium in which we exist”.
Alexander Lowen, The Voice of the Body.
Recently I had an interesting discussion with the head of a young sport-tech company which produces wearable devices for measuring breathing during exercise. These devices are T-shirts or vests with sensors which can extrapolate ventilation parameters from the chest movements. Additionally, the company suggests test build in phones and sports watches software which can define ventilation threshold from this data.
It happened that during my study at the University of Exeter, my fellow students and I made research on ventilation and lactate thresholds, and I still have some experimental data from that time. I did not pay much attention to ventilation since then because its testing was available only in laboratories and had little practical application in everyday coaching. That may change now when new technology arrives.
So, I used this opportunity to revisit our research and to make literature analysis with the aim to increase my knowledge about breathing during exercise. In this article I will not discuss how reliable the device is technically. Honestly, I did not test it. Instead, the topic of this work is the scientific rationale of its use in practical coaching.
What does a coach need?
To build up and maintain the training process the coach needs three basic things:
To prescribe (exercise)
To monitor (workload)
To evaluate (progress)
To help with these tasks, coaches and sports scientists can make physical and physiological measurements.
For many years physical monitoring and testing are traditionally used in the field. Today, due to developments in technology, a vast amount of physical information became available for coach. At the same time, the collection of physiological data is often more complicated and requires laboratories.
Probably the only physiological measure that from the old time is always at hand is heart rate ( HR). Without doubts, it is an essential parameter in physical activity. Contemporary technology allows continuous HR measure during exercise, analysis of intensity zones, HR recovery , and HR variability.
It has significant limitations, however. First of all, HR depends on many influences unrelated to physical workload. Secondly, during activity, it has a delayed period and sometimes lags behind changes in intensity. Finally, it doesn’t inform about stroke volume, which can be different in different forms of activity.
For more detailed analysis for implementations of HR measurements see the article.
Another physiological measure which coach can use in the field is blood lactate (BL). Now portable and affordable BL analysers are available. However, this method is invasive ; thus, perhaps you are not going to bleed your athletes too often.
Due to BL is an indirect measure of oxygen insufficiency and muscle acidosis, you should take its reading with caution (Robergs, Ghiasvand, & Parker, 2004). Appearance of lactate in blood has a significant delay; it does not precisely reflect lactate in muscles and depends on glycogen stores. So it does not precisely indicates the strain of exercise, especially in game sports. Moreover, one cannot trust absolute BL values. They can vary considerably at exhaustion or thresholds in different subjects. For example, low BL values at exhaustion is a typical picture for endurance athletes. In our experiment also; some participants were exhausted with lower BL concentrations than others, despite the better performance.
Considering all above, another non-invasive, mask-free and easy to implement ( just put your vest on) physiological measure may be beneficial. However, to understand how we can use this “new” data, we first have to talk about ventilation.
Ventilation in exercise.
Breathing is fundamental for all living things. Thus humans inherited it from our evolutionary predecessors with all its “illogical” complications in regulation, safety mechanisms, and multifactorial influences.
Though basically, the task is simple — to supply oxygen and to remove CO2.
Interestingly, despite the simplicity of ventilation (Ve) goals and all our contemporary knowledge, we still don’t understand how exactly the body detects changes in requirements and regulates breathing. All attempts to find one universal mechanism failed. It looks like there is multifactorial, redundant regulation with many interacting influences.
Ventilation is so crucial for survival that overlapping feedforward and feedback signals are used. It is regulated by central (brain) commands, afferent input from locomotor muscles, impulses from peripheral and central chemoreceptors, changes in core temperature and blood flow. You name it. All these mechanisms complement and interact with each other to ensure that even if for some reason, some of them fail, breathing can still cope with demands. For readers who want to learn more about the regulation of ventilation and to appreciate its complexity, I recommend excellent review “Control of Breathing During Exercise”(Forster, Haouzi, & Dempsey, 2012).
Measuring ventilation in a laboratory, we can find its mechanical parameters: volume, tidal volume (TV) and breath frequency (BF) as well as its physiological values: O2 consumption and CO2 removal.
Ventilation vests can give us only mechanical data.
Hyperventilation.
So let’s have a look at what happens with ventilation during incremental exercise or test.
In the beginning, everything doesn’t look complicated; ventilation increases following metabolic rate — linearly with O2 consumption and CO2 production. However, as exercise progress and intensity increases, Ve accelerates and departs from linearity with O2 (picture 1). It is important to note that it is not that O2 consumption slow down, it is Ve which accelerates. This “hyperventilation” or more exactly “exercise-induced hyperventilation” is not the same as pathological hyperventilation in unhealthy population. On the contrary, it is quite normal. So why do we need to breath more than oxygen can be utilised? The usual explanation is that we still need to remove CO2 which production increases more than O2 consumption.
Picture 1. Ventilation against VO2
Ventilation increases linear to VO2 until some point (threshold) when it accelerates.
From where “additional” CO2 may come?
The common explanation is that it comes from bicarbonate (HCO3) buffering of lactic acid. To prove that, a group of scientist from our university increased bicarbonate buffering by administrating dichloroacetate (Wilkerson, Campbell, Blackwell, Berger, & Jones, 2009). That, indeed decreased lactate and ventilation during sub-maximal intensities (not at maximal, however) .
Another research group administrated sodium bicarbonate intravenously and achieved delay in hyperventilation albeit could not prevent it (T. Meyer, Faude, Scharhag, Urhausen, & Kindermann, 2004).
However, some scientists do not support this theory. They pointed out that HCO3 is not the primary buffer, and it does not produce additional CO2 because bicarbonate formation uses CO2, which is already in the blood thus the reverse decomposing does not produce extra carbon dioxide. Rather a hyperventilation itself causes excessive CO2 washout, which is a well-known phenomenon. (Hopker, Jobson, & Pandit, 2011; Péronnet & Aguilaniu, 2006).
So if the additional CO2 is not the cause but instead the effect of hyperventilation what is the reason for latter then?
An alternative explanation is that ventilation may increase due to an accumulation of metabolites in the blood (e.g., potassium ions), increasing the perceived difficulty of exercise, increase in venous flow and impairment in gas exchange in lungs (Forster, Haouzi, & Dempsey, 2012; Mateika & Duffin, 1995).
Well, it’s beyond my expertise to judge on this topic.
I just can say for sure that at some point Ve and CO2 start to increase faster than O2. Extra CO2 may be produced by HCO3 buffering and/or increasing washout from the blood due to hyperventilation.
Deviation from CO2.
Sometime later, as intensity progresses, Ve deviates from CO2 as well. Again, CO2 production continues to rise; however, Ve accelerates even faster. The usual explanation is that buffering cannot cope with lactate production anymore and acidosis occurs. That gives a signal to chemoreceptors to increase ventilation.
Well, it’s unlikely so simple.
Hyperventilation at heavy intensity occurs even without acidosis. For instance, peripheral chemoreceptors, react not only on H ions but on many other metabolites including norepinenephrine and potassium. Increasing core and hypothalamus temperature, afferent signals from fatigued muscles and increased central efferent drive to them — all of these have a potential effect on hyperventilation (Forster, et al., 2012).
At least to some extent, hyperventilation may be associated with growing difficulty in gas exchange in the lungs. Increased speed of pulmonary blood flow leaves less time for gas exchange in alveoli. Hyperventilation may occur, including for this reason and facilitates gas exchange. At first, this leads to Ve rise disproportionally relative to VO2 and for some time CO2 removal can keep pace with ventilation due to CO2 exchanges easier than O2. When intensities increases further and time for exchange becomes even shorter, CO2 removal begins drag behind as well (Hopkins, 2019).
As we can see, regulation of ventilation is really complicated. I can finish “Ventilation” section with the conclusion that:
1. Ventilation possibly is a universal indicator of difficulty of the exercise. It integrates different psychological, locomotor, and biochemical signals. Perhaps it is why some authors argue that breathing is strongly correlated with another integrated measure — rate of perceived exertion (Nicolò, Marcora, Bazzucchi, & Sacchetti, 2017).
2. After some point during incremental exercise, ventilation increases faster than O2 utilisation and, later, even faster than CO2 production. It seems that this deviation from linearity with metabolic rate indicates an increase in the load on homeostasis. However, the mechanism of such “hyperventilation” is not yet completely understood.
Thresholds.
The concept of thresholds is fundamental to the physiology of exercise and coaching. Thresholds are boundaries that divide the intensity into areas with different time-limit for exercise. It is believed that existence of “global” physiological differences between domains emphasise and justify such a division.
Thresholds have a lot of different names as well as different concepts are used to explain them. Despite that , in my opinion, the idea is simple:
The first threshold represents border below which little changes in homeostasis occur; thus exercise may be maintained theoretically infinitely.
The second threshold is the highest intensity where changes in homeostasis can stabilise for a while; thus work in this domain can continue, though not infinitely, but relatively long (approximately one hour at threshold).
The third is the lowest intensity where oxygen utilisation reaches its maximum; thus, after that further increase in intensity is possible only anaerobically. Work at this threshold due to rapid disturbance of homeostasis is possible only for 5-10 min.
Respiratory and lactate thresholds.
Whereas the last threshold—VO2max provokes less controversy, the definition of first and second remains debatable.
They have different names, for example, aerobic and anaerobic, lactate and lactate turn point, ventilatory and respiratory compensation point and so on. They may be determined physiologically like, for example, maximal lactate steady state (MLSS) or mathematically — Critical Power (CP).
I have found excellent paper: “Methods to determine aerobic endurance” (Bosquet, Léger, & Legros, 2002) with a detailed description of thresholds their testing and practical applications. I highly recommend it.
Traditionally, the physiological determination of the first and second threshold is based on lactate and ventilation measurements.
For a long time, it is discussion whether lactate and ventilation thresholds are connected with each other.
It looks like they are not connected by direct cause-effect relationship (Svedahl & MacIntosh, 2003).
We are not breathing harder just because of lactate production. Instead they are different indicators of the same process — destabilisation of homeostasis (Robergs, Ghiasvand, & Parker, 2004) . Close analogy may be heat and smoke detectors of fire. They are both caused by the same event nevertheless they use different types of input.
The different nature of ventilation and lactate thresholds is highlighted by the fact that some exercise interventions influence them differently. For instance, breathing, as a universal indicator of difficulty, is effected by exercise-induced muscle damage (ventilation threshold happens earlier) whereas lactate threshold remains unchanged (Davies, Rowlands, Poole, Jones, & Eston, 2011; Burt, Lamb, Nicholas, & Twist, 2012).
So, what they really are?
Well, in my opinion, the very concept of the threshold needs more clarification. In essence, a threshold means a certain point where or when dramatic changes occur. It is like a cliff edge. You’re fine before that and dead after. However, human physiology operates with ranges of norms and gradual curves of changes, rather than abrupt edges. Some physiological parameters are more strictly regulated, some are relatively loose. But they are never fixed numbers. Thus the borders between domains are quite blurry and indicate tendency rather than “fait accompli”.
Considering ventilation and lactate thresholds I think that coaches perhaps do not need to know in depth its nature. Instead they may benefit from knowing the intensity “where fire may occur” — moment when metabolites production begins to exceed athletes ability to clean and tolerate them. This is not a fixed number but rather a probability which depends not only on fitness level but also on exercise mode, environmental conditions, and athlete’s current form. Nevertheless, approximation of this area may be useful for training and evaluation of progress.
In respiratory testing usually (not always) two ventilation thresholds are defined.
They are based on the phenomena which I already discussed above:
The 1-st threshold represents Ve departure from O2 consumption: Ve/VO2 goes up (Ve/VCO2 should remain flat).
The 2-nd indicates Ve departure from CO2 production: Ve/VCO2 goes up (Picture 2).
Picture 2. Determination of ventilation thresholds.
Our experiment.
Six subjects performed incremental stepwise cycle ergometer test twice. Warm up: 4 min – 50 W. After that increase 30 W every 3 min till exhaustion.
Results split participants into three different groups.
One subject was fatigued very quickly, three others finished at the same intensity stage with each other ( though spent different time in it) and two stages above him. Two best performers managed one stage more where the champ exercised one minute longer than runner-up.
We can see that ventilation can quite clearly distinguish between groups. For less fit participants ventilation curve accelerates (goes up) earlier (picture 3).
Picture 3.Ventilation during cycle ergometer test.
Number means the place taken in test (best – 1; last – 6).
However this separation happened relatively late, at the beginning everybody breathed basically the same. This is due to the fact that before the threshold, ventilation increases linearly with metabolic rate — O2 consumption (Hopker, Jobson, & Pandit, 2011). The latter increases with the same rate with intensity and basically identically for all participants (working economy were probably the same for all of us on a bike). After threshold, growing influence of factors discussed in “Ventilation” section causes departure of breathing from linearity with VO2 and separation participants into different “breathing groups” (picture 4).
Picture 4. Ventilation and oxygen consumption
VO2 remained basically the same for all participants until very late stages of testing. This was due to fact that oxygen cost of exercise was identical for all and increased in proportion to the external workload. This does not apply to breathing which at some point begins to reflect differences in internal workload in dependence on fitness. Vertical line shows time-point when ventilation separates five participants into two fitness groups despite the fact that their oxygen consumption still remains the same.
Respiration, perhaps was not so sensitive for separation participants within the same fitness group.
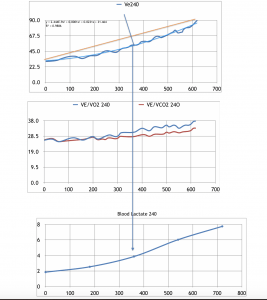
Breathing efficiency (Ve/O2 and Ve/CO2) followed ventilation pattern, illustrating that hyperventilation leads to a decrease in efficiency of oxygen consumption and later (and to a lesser extent) less efficient carbon dioxide removal (picture 5).
Picture 5. Time-course of ventilation and breathing efficiency.
Upper panel – Ve; middle – Ve/VO2; low – Ve/VCO2
Determination of thresholds with mechanical ventilation data.
Vests do not provide O2 and CO2 parameters; therefore, we cannot determine thresholds based on the ratio of Ve / VO2 and Ve / VCO2. We only have the Ve curve, and we need to define the threshold points on it. Where to choose?
First of all, I think that although some scientists are trying to determine two thresholds on the breathing curve, from a coaching perspective and for practical reasons, one is enough.
It should be some point after which rate of breathing accelerates, exercise becomes challenging, and its termination is looming. Training helps an athlete to exercise at such intensity longer and/or to move this border higher.
Secondly, as I said before, in reality there are no “cliff edge” points in ventilation. The curve line is smooth, and the concept of a threshold is a kind of abstraction. Therefore, you need to find some logic to justify your choice of a specific point for threshold. This choice may be based on intuition or math.
Visual methods.
Example of intuition is a visual approach.
Its aim is to find a point where the curve changes its steepness.
For example, the bi-line method divides the curve into two parts and builds best-fit straight lines for each section. It is assumed that the intersection of these lines is the threshold (picture 6).
Picture 6. Bi-line method.
The problem with this method is that the description of the curve with the straight lines is an approximation.
D-max visual method defines threshold as the furthest point on the curve from a line which connects the start and the end points of the test. Again, the assumption is that curve accelerates upwards from here (picture 7).
Picture 7. D-max method.
Ventilation is represented by polynomial function. AB line connects start and end points of the test. D-max is point on the curve furthest from line AB. Line a is tangent to the curve in point D-max and parallel to line AB.
Math.
Software cannot use intuition; instead, it implements math.
As an example, I describe mathematical logic behind the D-max method.
The software calculates a polynomial function for the ventilation line and a linear equation for the line AB.
The slope of line AB, which is a coefficient in linear equation, represents the average rate of increase in ventilation between A and B points. Point D-max on the curve is a place where line a, tangent to the curve (picture 7), is parallel to the line AB. Mathematically this means that derivative in point D-max is equal to the coefficient in the line AB equation.
Hence at point D-max speed of increase in the rate of ventilation is the same as test average . For example, if during the test Ve increased from 5 l/min to 105 l/min for 25 min, the average increment is 4 l/min. It is the same at D-max point. Before this point, increment is less than average after this point, it is higher. This may be good logical reason for choosing D-max method for threshold definition.
Example for participant R (data for calculation are taken after warm-up) :
3-d order polynomial function for ventilation: y= 3.072E-8x3– 2.407E-5x2+0.0324x+28.664
Linear equation for line AB: y=0.0689x + 25.6
Derivative for polynomial : 9.216E-8x2 -4.814E-5x-0.0324
In point D-max derivative is the same as coefficient for line AB ( 0.0689)
Thus we have: 9.216E-8x2 -4.814E-5x-0.0324=0.0689
x=943
D-max point is 943 seconds after warm up (4 min) or 1183 seconds from the start of the test.
Well, life is not pure math.
The fundamental and possibly unavoidable problem is that choosing the average ventilation increment rate as the threshold point has a mathematical reason but not a physiological one. For example, this point can be close to Ve/VO2 take off, but not exactly and not always.
This is clearly demonstrated by our most unfit participant (picture 8). His “physiological problems” reflected in the increase of Ve/VO2 and inflection of BL curve started long before his ventilation reached mathematical average (D-max threshold). .
Picture 8. D-max point, breathing efficacy and blood lactate for participant who took the six place.
Data is shown after 240 seconds of warm-up.
For the champion, the D-max point perhaps coincides or slightly precedes with the onset of significant changes in BL accumulation and respiratory efficacy (picture 9).
Picture 9. D-max point, breathing efficacy for participant who took the first place.
Another problem with D-max method is the choice of start and end point for line AB. This choice influences the slope of the line, thus the average speed of the function. For example, when choosing a starting point, you should think about whether or not to include a warm-up period when the ventilation rises initially, but usually stabilises after. Some authors suggest choosing a starting point only when the parameter begins to grow consistently.
There is less problem with the endpoint—you may choose it where exercise is finished, and ventilation reaches its maximum. However, you have to be sure that participant “gives his/her all.” Additionally, the endpoint may be influenced by test design ( I will talk about this later).
After trying different approaches, I suggest to draw the line from the beginning of the incremental part of the test, after warm up, and to the maximum in achieved Ve.
From my point of view, although ventilation curve reflects “objective” physiological events, the choice of D-max point on it remains “subjective” and depends on the researcher. I gave so detailed description of D-max method in order to show that this is just abstract representation of arbitrary threshold. Nothing ” physiologically special” happens at this mathematically derived point.
Basically, you can choose another method, point or reason. D-max method is not more “scientific” than other mathematical and intuitive approaches though it is not a bad choice either.
Testing.
Usually, though not always, researches use incremental tests to find out thresholds. The increment may be progressive or stepwise with different steepness.
The rate of increase in intensity dramatically influences the result.
For a review see article “Incremental Exercise Test Design and Analysis Implications for Performance Diagnostics in Endurance Athletes”(Bentley, Newell, & Bishop, 2007).
Progressive incremental test.
A relatively quick test with progressive increment is more common for VO2 max testing.
Indeed, when we are interested in some maximal values, like in this case, we probably just need quickly to reach these values without spending time on particular stages.
If we consider the physiological value of VO2 max, expressed in litres of O2, then it is some kind of ceiling which is always the same (I am not going to overload reader with “slow component”).
However, when VO2 max is expressed as the intensity at which it happened, for example, in speed units, it will not be the same in different tests. A subject may reach VO2 max at a lower speed if the test is longer (less increment).
Stepwise incremental test.
When we are interested in transitional parameters, like lactate/ventilation thresholds, we probably want to find more precisely where changes occur. If intensity increases rapidly and progressively, we may just rush by threshold point because the parameter of interest has no time to react.
Thus stepwise increase is more common in threshold testing.
Stage duration and the step of increase greatly influence the result in lactate and ventilation threshold testing. This makes sense: If a subject spends more time at pre-threshold intensities, the accumulation of by-products will be already significant, and threshold will happen at lower intensity compared to a faster increase and a shorter test.
Usually in BL protocol stage duration is more than 3 min with increase 1km/h per stage on treadmill or 30W on a bike. The rationale is that lactate needs significant time to make its way from working muscles to the blood.
Respiration reacts significantly faster than lactate, so it is why some researchers consider spending time on the stages unnecessary. Well, as I said before, breathing has multiple regulatory signals. For example Nicolo et al. suggested that Central command in ventilation rapidly reacts on changes in intensity (and this is reflected in BF) whereas reaction on metabolic changes is much slower (reflected in TV) (Nicolò, Marcora, Bazzucchi, & Sacchetti, 2017) .
Though this explanation may be an oversimplification, we still have to take into account delay in reaction on metabolic changes thus it is better to give time for ventilation to show its behaviour and to stay for a while on a particular stage. Additionally, this may help to reduce noise from accidental, unusual breathing patterns.
However, whatever design we choose it is important to remember that:
Threshold speed or power found in a particular test is not the universal value. It is specific for this test design.
Despite the results may be different, they still reflect the same physiological processes. Thus they have a good correlation with each other and with some aspects of performance.
Therefore, if we are consistent in test design, we can take its results for evaluation of improvement and for comparison between subjects.
However, test results are not the ultimate values for exercise prescription.
What test design can I suggest for determining Ve threshold with the vest?
The company suggests an incremental test with a progressive increase of 1 km/h in 1 min. As I already mentioned, it is rather VO2 max test design. The advantage which attracts company is that it is relatively short ( approximately 10 min without warm up).
For the reasons that I already discussed above, I tend to be in favour of longer stepwise test.
Subject does not need to spend 3 min on stage as in BL testing, and step increment may be smaller for more precise threshold definition. Thus, probably, 1 min stage with increment 0.5 km/h will be worth to try. That gives us approximately 2/3 duration of BL testing ( approx 20 min, including 4 min warm-up).
Whatever test we use, we should be consistent, careful, and use common sense while evaluating results.
The need for sub-maximal ventilation testing.
You cannot torture athletes with maximal testing too often. They have no time for it, and they don’t like it (especially sport games athletes). So can ventilation give us reliable information about athletes fitness without the need of exhaustive run?
I think that breathing during constant-speed, sub-maximal run can provide a solution.
I have found the research where authors compare ventilation parameters at a fixed speed of 16 km/h before and after training to assess the improvements in fitness (Di Paco, Dubé, & Laveneziana, 2017). The idea may be useful. In their experiment, this speed was transitional in maximal testing. It may be lower if athletes spend more time at it (e.g.5 min).
Running at such speed is easier for fitter athletes or when they are in better shape; thus, their breathing rate should be lower than for unfit subjects or bad form. Consequently, this run can possibly distinguish improvements in fitness after training or fluctuations in form.
So at which speed this constant run should be set?
Well, as it was discussed, at speeds below threshold Ve mostly reflects the metabolic rate and probably is not informative about the disturbance in homeostasis; thus, we need some at or over threshold intensity.
We are probably have to challenge an athlete for evoking noticeable changes; however, we don’t want to exhaust him/her. Thus, perhaps 5 minutes running at speed not much higher than the ventilation threshold (let’s say D-max point) should be appropriate. If you don’t know threshold speed, set the test at around 40-45% of the maximal speed (Billat, 2001).
So test design maybe following: 3 min warm-up at low-intensity run. Immediately after, 3 min incremental part towards aimed steady pace intensity. The increment may be fast – we are not interested to stay for a long in transition zone. So, let’s say 1 km/h every minute. After that 5 min at a constant speed. Lower than usual Ve during this 5 min — improved fitness. Higher— impaired fitness and/or current form.
Example:
Athlete with approx max speed 35 km/h. Aimed constant speed – 15 km/h.
1. 3min -10 km/h constant speed.
2. 3 min increment from 12 to 14 (1km/h every min).
3. 5 min at 15 km/h.
Overall test duration – 11 min.
Using ventilation data for training.
1. Prescription
Traditionally track and field coaches prescribe training based on speed in particular distances. For example, interval’s speed in interval training 4 x1000m with 1.5 min passive rest may be set at speed on 3000 m.
We have to recognise that such a practical approach proved to be successful over the decades of progressive improvement in athletics results.
Theoretically, threshold speed may be extrapolated from personal best results on some distances. However there are no consensus among sport scientists speed on which distance is a threshold speed. At least in part this is due to the fact that threshold itself is defined differently.
Veronique Billat , one of the leading researcher in physiological thresholds, suggested that at MLSS which to some extent is lactate analogy of “our” ventilation threshold, good level athletes can run around one hour thus it may be their personal best on 10 miles—half-marathon(Billat, 2001). My teacher at the University of Exeter Andrew Jones argues that for elite runners, it is a marathon speed (Jones & Vanhatalo, 2017). Mathematically derived “Critical speed” usually is close to 10 km result for competitive runners.
So, does threshold speed, found with ventilation vest, gives us some advantage?
Apologists of physiological testing may say that ventilation test gives “objective” value which reflects physiological processes whereas speed on a distance is “subjective” result. Well, athletic coaches may argue that speed reflects athletes physiology as well, and that ventilation threshold depends on test design and gives you different threshold speeds in different tests.
Well, this is true, and of course, I am not going to teach athletic coaches. I already said that the ventilation threshold expressed as speed/power is not universal value for reference point. However, as correctly pointed out Buchheit and Laursen, speed on the set of distances may be well-known for experienced track-and-field athletes, whereas their game-sports colleagues have less knowledge about that. And they may be not used to run long distances. Thus ventilation threshold may be some useful addition to traditional prescription methods, especially when the improvement of physiological quality is the aim , not an improvement on a particular distance (Buchheit & Laursen, 2013).
Very important however, to be consistent in the test design and method for threshold definition.
2. Evaluation of internal workload.
Let’s take an example when you are doing tempo-run training, for instance 2x 25 min run at your threshold speed. You have found this speed during the test in laboratory, or with ventilation vest test, or just take your personal best in 10 km. Usually, it is not an easy running, but today it feels ok. Rate of perceived exertion (RPE) is lower. After training, you may check your HR and ventilation data. In my opinion, lower than usual breathing rate may be taken as evidence that today running was indeed easier. Lower HR may give further support for that, but, even if it was not lower, you still can trust your feelings (RPE) and ventilation. If this pattern repeats, maybe it is time to move your threshold speed up.
Possibly ventilation may be used for assessing internal workload in session. For example, time spent in high-intensity zones. Currently we are using HR for that. As I mentioned above, HR has its limitation, especially for assessing intermittent activities. BL measures are impractical. Some sports practitioners start to use RPE for assessing internal workload. Perhaps ventilation which combines universality of RPE with a physiological basis of HR and BL may be a suitable candidate. However, the question is how it can be technically reliable in-game sports where intense and sporadic body movements may spoil ventilation reading from the chest.
3. Assessing progress.
Shifting threshold to the right on intensity scale ( towards higher intensity) may tell us about general progress in fitness. Ventilation test with the vest is easier to implement than BL testing. However, both tests are maximal so you cannot perform them too often.
Possibly sub-maximal, steady-pace test described above may be an alternative.
4. Distinguishing between athletes.
Fitter athletes should have a ventilatory threshold at higher intensity; thus, this vest can be useful to distinguish between athletes.
Though our study seemingly supports this idea, ventilation, however, could not distinguish differences in fitness between athletes within the same fitness category.
I think this is due to some individual variability in the regulation of breathing, which is independent of fitness level.
It is similar to HR at sub-maximal run. It can clearly distinguish between athletes and non-athletes (athletes have significantly lower HR); however, it is not so informative for comparison of the same level subjects.
Additionally, vest unlikely give you reliable absolute values of ventilation, because it “does not know” tidal volume in absolute numbers. It extrapolates it from the amplitude of chest movement. Whereas it is acceptable when compare athlete with him/herself, it may be imprecise when compare with others.
5. Evaluating current form.
One of the biggest challenges in training is evaluating athletes current conditions. Is he/she feeling ok today? Are they ready for a hard workout or it is better to give them easy training?
Although RPE is always at hand, it is still subjective, and the need for objective assessment exists.
That is where physical/physiological testing may help.
This testing needs to be short and sub-maximal because the decision should be made quickly and the test load should not intervene with planned training load.
One of the candidates is the countermovement jump. It combines strength and neuromuscular coordination, and, to some extent, can assess current conditions.
Another idea is to use HR during sub-maximal 5 min run incorporated into warm up. Higher than usual HR may tell us that athlete is tired today (Buchheit, 2014).
Can ventilation be useful in this aspect?
In our experiment, one participant performed better in the second test than in the first. He managed to spend 2 min more on his last intensity stage. Tests were separated by just two days; thus, no training effect was possible. Of course, there may be an effect of “learning” the test, but this is unlikely because it is technically simple and he knew it very well during undergraduate study at the same Uni. Another reason may be a lack of motivation in the first test, but high blood lactate (7.3 mmol/L) indirectly shows that he “gave it all.” So we may suppose that for some reason he felt better on the second occasion and improved his result.
Was that somehow reflected in his ventilation data? Let’s have a look at picture 10.
Picture 10. Ventilation in two tests for participant A.
The persistent difference in ventilation started to be evident after 800 sec . It was one step below his Ve threshold calculated by the D-max method (983 first test; 994-second test). The gap remained pretty stable (4-5L/min) until new increase in intensity, one step above D-max point, when it widened to 12 L/min and stayed at this level almost to the end of the test 1.
Thus, with some caution, I can suggest that ventilation may be informative for evaluating current form.
Sub-maximal, constant-speed ventilation test may be used for such assessment. However, due to it is still relatively intense it would be impractical to use it every day. Perhaps we can use it for assessing current form at the beginning of the week training cycle.
Conclusion.
Ventilation is regulated by multiple feedforward and feedback signals. It reflects neuromuscular, psychological and biochemical strain of exercise. Thus it may give integrated picture of difficulty of exercise.
Ventilation is more informative after threshold where it starts to reflect disturbance in homeostasis and difficulty of exercise. At low intensities ventilation mostly reflects metabolic rate and is mainly proportional to the workload; therefor is less informative.
Although the ventilation curve reflects physiological processes, the determination of the threshold(s) on it without the presence of physiological data (for example, VO2 and VCO2) has a limited physiological basis. Rather, it is based on mathematical or intuitive reasoning and depends on the method. However, this can still be useful if scientists are consistent in their choice of methods.
Test with fast and progressive increase of intensity, applicable for VO2 testing, may significantly overestimate ventilatory threshold compare to generally accepted practical criteria ( speed which can be sustained approximately 1 hour) . Therefore, for testing with ventilation vest, I tend to recommend stepwise and slower increase with stage duration 1min and step 0.5 km/h.
Ventilation during sub-maximal, constant-speed test may be helpful for evaluation fitness level and current form. This constant- speed should be set at or slightly above ventilatory threshold.
In summary: a ventilation vest can be a useful tool for assigning, monitoring and evaluating training load, current form and progress.
Final remarks.
I am writing articles because it is my way to comprehend things. I do not aim publishing in journals. My opinion, expressed in this work, is not based on rigorous research , thus some of my conclusions and suggestions may be incorrect. At the end of the day I am more coach than scientist.
I understand that presented work is definitely not enough academic for serious scientists and perhaps is too difficult reading for some of practitioners.
However it is, in my opinion, important for sports people to understand scientific basis underlying the new tech devices, to know its limitations and to implement them wisely.
So I will be glad if this article can provide at least a little help to coaches and athletes.
References.
Bentley, D. J., Newell, J., & Bishop, D. (2007). Incremental exercise test design and analysis. Sports Medicine, 37(7), 575-586.
Billat, L. V. (2001). Interval training for performance: a scientific and empirical practice. Special recommendations for middle- and long-distance running. Part I: aerobic interval training. Sports Med, 31(1), 13-31.
Bosquet, L., Léger, L., & Legros, P. (2002). Methods to determine aerobic endurance. Sports Medicine, 32(11), 675-700.
Buchheit, M. (2014). Monitoring training status with HR measures: do all roads lead to Rome? Front Physiol, 5(73).
Buchheit, M., & Laursen, P. B. (2013). High-intensity interval training, solutions to the programming puzzle: Part I: cardiopulmonary emphasis. Sports Med, 43(5), 313-338.
Burt, D., Lamb, K., Nicholas, C., & Twist, C. (2012). Effects of muscle-damaging exercise on physiological, metabolic, and perceptual responses during two modes of endurance exercise. Journal of Exercise Science & Fitness, 10(2), 70-77. doi: https://doi.org/10.1016/j.jesf.2012.10.003
Davies, R. C., Rowlands, A. V., Poole, D. C., Jones, A. M., & Eston, R. G. (2011). Eccentric exercise-induced muscle damage dissociates the lactate and gas exchange thresholds. Journal of Sports Sciences, 29(2), 181-189.
Di Paco, A., Dubé, B.-P., & Laveneziana, P. (2017). Changes in Ventilatory Response to Exercise in Trained Athletes: Respiratory Physiological Benefits Beyond Cardiovascular Performance. Archivos de Bronconeumología (English Edition), 53(5), 237-244.
Forster, H. V., Haouzi, P., & Dempsey, J. A. (2012). Control of breathing during exercise. Compr Physiol, 2(1), 743-777.
Hopker, J. G., Jobson, S. A., & Pandit, J. (2011). Controversies in the physiological basis of the ‘anaerobic threshold’and their implications for clinical cardiopulmonary exercise testing. Anaesthesia, 66(2), 111-123.
Hopkins, S. (2019). Pulmonary diffusion limitation, V̇ /Q̇ mismatch and pulmonary transit time in highly trained athletes during maximal exercise.
Jones, A. M., & Vanhatalo, A. (2017). The ‘critical power’concept: applications to sports performance with a focus on intermittent high-intensity exercise. Sports Medicine, 47(1), 65-78.
Mateika, J. H., & Duffin, J. (1995). A review of the control of breathing during exercise. Eur J Appl Physiol Occup Physiol, 71(1), 1-27.
Meyer, T., Faude, O., Scharhag, J., Urhausen, A., & Kindermann, W. (2004). Is lactic acidosis a cause of exercise induced hyperventilation at the respiratory compensation point? British Journal of Sports Medicine, 38(5), 622-625. doi: 10.1136/bjsm.2003.007815
Meyer, T., Lucia, A., Earnest, C. P., & Kindermann, W. (2005). A conceptual framework for performance diagnosis and training prescription from submaximal gas exchange parameters-theory and application. International journal of sports medicine, 26(S 1), S38-S48.
Nicolò, A., Marcora, S. M., Bazzucchi, I., & Sacchetti, M. (2017). Differential control of respiratory frequency and tidal volume during high‐intensity interval training. Experimental Physiology, 102(8), 934-949.
Péronnet, F., & Aguilaniu, B. (2006). Lactic acid buffering, nonmetabolic CO2 and exercise hyperventilation: a critical reappraisal. Respiratory Physiology & Neurobiology, 150(1), 4-18.
Robergs, R. A., Ghiasvand, F., & Parker, D. (2004). Biochemistry of exercise-induced metabolic acidosis. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 287(3), R502-R516.
Svedahl, K., & MacIntosh, B. R. (2003). Anaerobic threshold: the concept and methods of measurement. Canadian journal of applied physiology, 28(2), 299-323.
Turner, D. L. (1991). Cardiovascular and respiratory control mechanisms during exercise: an integrated view. Journal of Experimental Biology, 160(1), 309-340.
Wilkerson, D. P., Campbell, I. T., Blackwell, J. R., Berger, N. J., & Jones, A. M. (2009). Influence of dichloroacetate on pulmonary gas exchange and ventilation during incremental exercise in healthy humans. Respiratory Physiology & Neurobiology, 168(3), 224-229.